Endosteal Dental Implant

What Is An Endosteal Dental Implant?
Endosteal Dental Implants stand as a revolutionary solution for restoring smiles and dental functionality. These implants serve as artificial tooth roots, offering a robust foundation for prosthetic teeth like crowns, bridges, or dentures. Unlike traditional removable dentures, endosteal implants are firmly anchored within the jawbone, mimicking the natural structure of teeth and providing a stable base for replacement teeth.
Endosteal implants consist of biocompatible materials such as titanium, which seamlessly integrate with the jawbone through a process called osseointegration. This integration ensures long-term stability and durability, allowing patients to regain confidence in their smiles and enjoy restored chewing ability.
Before deciding on whether Endosteal Dental Implant are right for you, there are some things you should know:
- Who Needs An Endosteal Dental Implant?
- What Are The Indications For Endosteal Dental Implant?
- What Are The Contraindications For Endosteal Dental Implant?
- What Are The Advantages Of Endosteal Dental Implant?
- What Are The Potential Risks Or Complications Of Endosteal Dental Implant?
- What Are The Alternative Treatments If I Do Not Choose Endosteal Dental Implant?
- How Much Do Endosteal Dental Implants Cost?
- What Are The Steps In The Endosteal Dental Implant Procedure?
- How Long Does Endosteal Dental Implant Last?
- What Are Common Problems With Endosteal Dental Implant?
If you have any further questions about Endosteal Dental Implant or other dental services offered at Atlas Dental, please contact us.
Free phone consultation
Have questions about Endosteal Implants? Schedule a free phone consultation with our Toronto dentist.
5 star google reviews
Our patients love us! See for yourself why people are choosing Atlas Dental in Toronto for Endosteal Implants.
Dental Implant Crown Emergency Service
Are you having trouble with your Endosteal Implant? Book an emergency appointment today.
Who Needs An Endosteal Dental Implant?
Endosteal dental implants offer a lifelike and durable solution for individuals facing tooth loss due to various reasons. If you find yourself in any of the following situations, an endosteal dental implant might be the ideal option to restore your smile and oral function:
- Missing Teeth: Endosteal implants are perfect for individuals missing one or more teeth. Whether the tooth loss is due to decay, trauma, or other dental issues, implants can fill the gap and provide a natural-looking replacement.
- Unstable Dentures: If you currently wear removable dentures and find them slipping or shifting uncomfortably while speaking or eating, endosteal implants can offer a stable alternative. Implant-supported dentures provide a secure fit, eliminating worries about slippage and enhancing overall comfort.
- Jawbone Health Concerns: In some cases, individuals may experience jawbone deterioration or loss of bone density, making traditional dental implants less viable. Endosteal implants, with their ability to integrate deeply into the jawbone, can often overcome such challenges, providing a strong foundation for replacement teeth.
- Desire for a Permanent Solution: Unlike temporary solutions like bridges or dentures, endosteal dental implants offer a permanent fix for tooth loss. Once integrated with the jawbone, these implants become a natural part of your oral anatomy, providing long-lasting support and stability for your prosthetic teeth.
- Improved Oral Health: By replacing missing teeth with endosteal implants, you can maintain proper dental alignment and prevent neighboring teeth from shifting out of place. This helps preserve overall oral health and prevents potential complications such as bite issues or gum disease.
Whether you’re missing a single tooth or need to replace an entire dental arch, endosteal dental implants provide a versatile and effective solution for restoring your smile and confidence. However, candidacy for implant treatment depends on various factors, including overall health, jawbone density, and oral hygiene habits. Consulting with a qualified dental professional can help determine if endosteal implants are the right choice for your specific needs. If you have further questions about Endosteal Dental Implant, please contact us.

What Are The Indications For Endosteal Dental Implant?
Endosteal dental implants are a versatile and effective solution for restoring missing teeth and improving oral health. Several indications may suggest that you are a suitable candidate for endosteal implant treatment. Here are some common scenarios where endosteal dental implants may be recommended:
- Single Tooth Replacement: If you are missing a single tooth due to decay, trauma, or other dental issues, an endosteal implant can provide a stable and natural-looking replacement. Unlike traditional bridges that require altering adjacent teeth, an implant-supported crown preserves the integrity of neighboring teeth while restoring the aesthetics and functionality of your smile.
- Multiple Teeth Replacement: Endosteal implants are also an excellent option for replacing multiple missing teeth. Whether you have consecutive missing teeth or several gaps throughout your dental arch, implants can support fixed bridges or implant-supported dentures, providing a comprehensive solution for restoring your smile and chewing ability.
- Denture Stabilization: If you currently wear removable dentures and struggle with issues like slippage, discomfort, or difficulty chewing, implant-supported dentures can offer a significant improvement in stability and function. By anchoring your dentures to strategically placed endosteal implants, you can enjoy enhanced confidence and comfort while eating, speaking, and smiling.
- Jawbone Preservation: After tooth loss, the underlying jawbone may begin to deteriorate over time due to lack of stimulation from tooth roots. Endosteal implants help preserve jawbone density by stimulating bone growth through osseointegration. This not only maintains the structural integrity of your jawbone but also prevents further bone loss and associated facial changes.
- Enhanced Stability and Function: Endosteal implants provide a level of stability and functionality that surpasses traditional tooth replacement options like bridges or dentures. Because implants are anchored directly into the jawbone, they mimic the natural structure of teeth, allowing for more efficient chewing and speaking and providing a more comfortable and secure fit for your prosthetic teeth.
- Improved Oral Health: By replacing missing teeth with endosteal implants, you can prevent potential oral health issues such as shifting of adjacent teeth, gum recession, and bone loss. Maintaining proper dental alignment with implants also facilitates easier oral hygiene practices, reducing the risk of gum disease and tooth decay in the long run.
If you experience any of the indications mentioned above or have concerns about tooth loss and its impact on your oral health and quality of life, consulting with a qualified dental professional is the first step toward exploring your options for endosteal dental implant treatment. A comprehensive evaluation will help determine if you are a suitable candidate for implant therapy and develop a personalized treatment plan tailored to your needs and goals. If you have further questions about Endosteal Dental Implant, please contact us.
What Are The Contraindications For Endosteal Dental Implant?
While endosteal dental implants offer numerous benefits for restoring missing teeth and improving oral health, certain factors may contraindicate their use in some individuals. Understanding these contraindications is essential for ensuring the success and longevity of implant treatment. Here are some common contraindications for endosteal dental implants:
- Poor Jawbone Quality or Quantity: Adequate jawbone density and volume are crucial for the successful placement and integration of endosteal implants. Patients with severe jawbone deterioration or insufficient bone volume may not have enough support for implant placement. In such cases, bone grafting or alternative treatment options may be necessary to augment the jawbone before implant surgery.
- Uncontrolled Systemic Conditions: Certain systemic health conditions, such as uncontrolled diabetes, autoimmune disorders, or bleeding disorders, can compromise the body’s ability to heal properly after implant surgery. Patients with these conditions may have an increased risk of implant failure or complications and may not be suitable candidates for implant treatment until their systemic health is adequately managed.
- Active Periodontal Disease: Periodontal disease, characterized by inflammation and infection of the gums and supporting tissues, can weaken the foundation for dental implants and increase the risk of implant failure. Patients with active periodontal disease may require periodontal treatment and maintenance before implant placement to ensure a healthy oral environment conducive to successful implant integration.
- Smoking or Tobacco Use: Smoking and tobacco use have been linked to impaired healing, decreased blood flow, and increased risk of implant failure. Nicotine and other chemicals in tobacco products can hinder osseointegration—the process by which implants fuse with the jawbone—and compromise the long-term stability of implants. Patients who smoke or use tobacco products may need to quit or reduce their usage before undergoing implant surgery.
- Immunosuppressive Therapy: Patients undergoing immunosuppressive therapy, such as chemotherapy or long-term steroid treatment, may have compromised immune systems, which can affect their ability to heal after implant surgery. Dentists may need to coordinate treatment with the patient’s healthcare provider and adjust the timing of implant placement to minimize the risk of complications.
- Pregnancy: Pregnant women are generally advised to avoid elective dental procedures, including implant surgery, during pregnancy due to potential risks to fetal development and the mother’s health. Implant treatment is typically deferred until after childbirth and the completion of breastfeeding to ensure the safety of both the mother and the baby.
Before undergoing endosteal dental implant treatment, it’s crucial to undergo a comprehensive evaluation with a qualified dental professional to assess your oral health, medical history, and suitability for implant therapy. By identifying and addressing any contraindications upfront, you can minimize the risk of complications and maximize the success of your implant treatment journey. If you have further questions about Endosteal Dental Implant, please contact us.

What Are The Advantages Of Endosteal Dental Implant?
Endosteal dental implants offer numerous advantages compared to traditional tooth replacement options like bridges or removable dentures. Understanding these benefits can help you make an informed decision about your dental treatment. Here are some of the key advantages of endosteal dental implants:
- Natural Look and Feel: Endosteal implants closely mimic the appearance and function of natural teeth, providing a seamless solution for replacing missing teeth. With custom-designed prosthetic teeth attached to the implants, you can enjoy a natural-looking smile and restored chewing ability, enhancing your confidence and quality of life.
- Long-Term Durability: Endosteal implants are designed to be a permanent tooth replacement solution, offering exceptional durability and longevity. With proper care and maintenance, implants can last for many years or even a lifetime, making them a cost-effective investment in your oral health and overall well-being.
- Improved Bone Health: Unlike traditional bridges or dentures, which rest on the gums or rely on adjacent teeth for support, endosteal implants stimulate bone growth and help preserve jawbone density. Through a process called osseointegration, implants fuse with the jawbone, providing stability and preventing bone resorption. This helps maintain facial contours and prevents the sunken appearance often associated with tooth loss.
- Enhanced Comfort and Stability: Endosteal implants eliminate the discomfort and inconvenience often associated with removable dentures, such as slippage, sore spots, and difficulty speaking or eating. By anchoring prosthetic teeth securely to the jawbone, implants provide stability and support, allowing you to enjoy a more comfortable and natural-feeling restoration.
- Preservation of Adjacent Teeth: Unlike traditional bridges, which require the alteration of adjacent teeth to support the restoration, endosteal implants preserve the integrity of neighboring teeth. This means that healthy teeth do not need to be filed down or compromised in any way, preserving their natural structure and minimizing the risk of future dental problems.
- Improved Oral Health: Endosteal implants support optimal oral hygiene practices by allowing for easy access to the surrounding gum tissue and neighboring teeth. Unlike removable dentures, which can trap food particles and bacteria underneath, implant-supported restorations can be brushed and flossed just like natural teeth, promoting better oral health and reducing the risk of gum disease and tooth decay.
- Restored Confidence and Self-Esteem: With endosteal implants, you can regain the ability to smile, speak, and eat with confidence, knowing that your replacement teeth are secure and stable. The natural look and feel of implant-supported restorations can boost self-esteem and improve overall quality of life, allowing you to enjoy social interactions and everyday activities without hesitation.
Endosteal dental implants offer a comprehensive solution for replacing missing teeth and restoring oral health and function. If you are considering tooth replacement options, consulting with a qualified dental professional can help determine if endosteal implants are the right choice for your individual needs and goals. If you have further questions about Endosteal Dental Implant, please contact us.
What Are The Potential Risks Or Complications Of Endosteal Dental Implant?
While endosteal dental implants are generally safe and successful for most patients, like any surgical procedure, there are potential risks and complications to consider. Understanding these risks can help you make an informed decision about undergoing implant treatment. Here are some potential risks or complications associated with endosteal dental implants:
- Dental Infection: Infection is a common risk following implant surgery, particularly if proper oral hygiene practices are not maintained during the healing process. Symptoms of infection may include swelling, pain, redness, or discharge around the implant site. Prompt treatment with antibiotics may be necessary to address the infection and prevent complications.
- Implant Failure: While rare, implant failure can occur if the implant does not successfully integrate with the surrounding jawbone or if osseointegration is disrupted during the healing period. Factors such as poor bone quality, smoking, uncontrolled diabetes, or inadequate postoperative care can increase the risk of implant failure. In some cases, failed implants may need to be removed and replaced with additional surgical procedures.
- Nerve Damage: During implant surgery, there is a risk of nerve injury, particularly in the lower jaw where the inferior alveolar nerve runs. Nerve damage may result in numbness, tingling, or altered sensation in the lips, chin, or tongue. While nerve injuries are rare, they can cause temporary or permanent discomfort and may require additional treatment to resolve.
- Gum Recession: Improper placement of the implant or inadequate tissue management during surgery may lead to gum recession around the implant site. Gum recession can expose the implant threads or restoration margins, compromising the aesthetics and longevity of the implant-supported restoration. Proper surgical technique and regular dental visits can help monitor and manage gum health following implant placement.
- Bone Loss: In some cases, bone loss may occur around the implant site over time, leading to instability or failure of the implant. Factors such as poor oral hygiene, peri-implantitis (inflammation of the tissues surrounding the implant), or excessive biting forces can contribute to bone loss. Regular dental check-ups and proper maintenance of oral hygiene can help prevent or mitigate bone loss around implants.
- Allergic Reactions: While rare, some individuals may experience allergic reactions to the materials used in endosteal implants, such as titanium or other metals. Symptoms of an allergic reaction may include swelling, redness, or itching around the implant site. Patients with known allergies or sensitivities should discuss alternative implant materials with their dentist.
- Sinus Complications: For implants placed in the posterior maxilla (upper jaw), there is a risk of sinus complications, particularly if the sinus cavity is breached during surgery. Sinus perforation may result in sinus infections, sinusitis, or discomfort in the nasal area. Proper preoperative assessment and surgical planning can help minimize the risk of sinus complications during implant placement.
Before undergoing endosteal dental implant treatment, it’s essential to discuss the potential risks and complications with your dentist and weigh them against the benefits of implant therapy. With proper planning, surgical technique, and postoperative care, the vast majority of patients can enjoy successful outcomes with endosteal dental implants. If you have further questions about Endosteal Dental Implant, please contact us.

What Are The Alternative Treatments If I Do Not Choose Endosteal Dental Implant?
If endosteal dental implants are not suitable for you due to various reasons such as medical conditions, anatomical constraints, or personal preferences, several alternative treatments are available to replace missing teeth and restore your smile and oral function. Here are some common alternative treatments to consider:
- Traditional Bridges: Traditional dental bridges consist of prosthetic teeth (pontics) anchored to adjacent natural teeth using dental crowns. Bridges are an effective option for replacing one or more consecutive missing teeth and restoring chewing ability and aesthetics. However, they require the alteration of healthy adjacent teeth to support the bridge, which may compromise their long-term health and integrity.
- Removable Dentures: Removable dentures are a non-invasive and cost-effective option for replacing multiple missing teeth or an entire dental arch. Dentures rest on the gums and rely on suction or adhesives for stability. While dentures can restore aesthetics and chewing function, they may feel less secure than implants and may cause discomfort or irritation to the gums over time.
- Resin-Bonded Bridges (Maryland Bridges): Resin-bonded bridges, also known as Maryland bridges, are a conservative alternative to traditional bridges that do not require the alteration of adjacent teeth. These bridges consist of prosthetic teeth bonded to adjacent teeth using metal or porcelain wings. While Maryland bridges offer a minimally invasive solution for replacing missing teeth, they may not be as durable or stable as implants.
- Flipper Dentures: Flipper dentures, also called temporary partial dentures, are removable prosthetic devices designed to replace one or more missing teeth on a temporary basis. These lightweight dentures are typically used during the healing period following tooth extraction or implant surgery. While flipper dentures provide immediate tooth replacement, they are considered a temporary solution and may require frequent adjustments.
Before deciding on a tooth replacement option, it’s essential to discuss your concerns, preferences, and treatment goals with your dentist. Together, you can explore the various alternatives and determine the most suitable treatment plan to restore your smile and oral function effectively. If you have further questions about Endosteal Dental Implant, please contact us.
Cost of Dental Implant
A Dental Implant often involves multiple components and fees including tooth removal (code 71201), the dental implant placement (79931), bone grafting (72421) and the dental implant crown (27215). Therefore, depending on your needs, the cost of a single tooth dental implant can range between $4165 to $5222. The codes relevant to dental implants in the Ontario Dental Association’s Suggested Fee Guide appear as follows:
Removals, Erupted Teeth, Complicated
- 71201 – Removals, Erupted Tooth, Surgical Approach, Requiring Surgical Flap and/or Sectioning of Tooth: $307
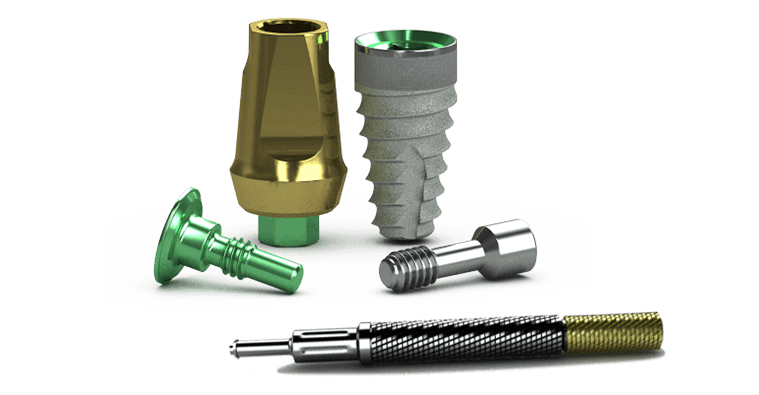
Implants, Osseointegrated, Root Form, More than one component
- 79931 – Surgical Installation of Implant with Cover Screw – per implant: $1785+ Dental Materials Expense (approximately $350)
Alveolar Bone Preservation – Allograft
- 72421 – First tooth: $450 + Dental Materials Expense (approximately $300)
Crowns, Porcelain/Ceramic/Polymer Glass Fused to Metal
- 27215 – Crown, Porcelain/Ceramic/Polymer Glass Fused to Metal Base, Implant-Supported: $1280 + Dental Lab Fee + Dental Materials Expense (approximately $750)
In Ontario, most dentists will provide basic dental surgery and restorative dental services consistent with the Ontario Dental Association’s Suggested Fee Guide, such as dental emergency examinations, dental x-rays and tooth extractions, to ensure fair and competitive treatment cost. The Ontario Dental Association’s Suggested Fee Guide is a proposed fee structure that dentists in Ontario may or may not follow. Please consult with your dentist about fees before going ahead with treatment.
Each dental implant surgery case is unique. Depending on your unique circumstance, implant surgery may be more difficult and more expensive if any of the following is required:
- CBCT scanning
- Computer guided implant surgery
- Immediate implant placement following tooth extraction
- Bone grafting to prevent bone loss
- Bone regeneration to grow new bone
- Simultaneous gum graft procedures
- Immediate tooth replacement at the time of surgery
- Sinus lifting procedures to raise the maxillary sinus floor
Dental Implant services are usually considered a supplementary service by dental insurance plans and may or may not be covered by your dental insurance. Be sure to find out from your dental insurance plan provider how much you are eligible for before going ahead with dental treatment. Your dentist can help you submit an predetermination to your dental insurance.
For patients without dental insurance, Atlas Dental is pleased to offer dental financing through Dentalcard. Affordable payment plans start at 7.95% for terms of 6 months to 6 years. To learn more about Dentalcard dental treatment financing, follow this link.
What Are The Steps In The Endosteal Dental Implant Procedure?
The endosteal dental implant procedure involves several stages, from initial consultation to final restoration. While specific steps may vary depending on individual patient needs and treatment plans, the following outlines the typical process involved in placing endosteal dental implants:
- Initial Consultation and Examination: The first step in the implant process is a comprehensive consultation with your dentist or oral surgeon. During this visit, your dentist will evaluate your oral health, medical history, and jawbone anatomy to determine if you are a suitable candidate for endosteal implants. X-rays, CBCT scans, or 3D imaging may be taken to assess bone density and identify potential anatomical challenges.
- Treatment Planning: Based on the results of the examination and diagnostic imaging, your dentist will develop a personalized treatment plan tailored to your specific needs and goals. This plan will outline the number of implants needed, their optimal placement positions, and any additional procedures, such as bone grafting or sinus augmentation, that may be required to ensure the success of implant treatment.
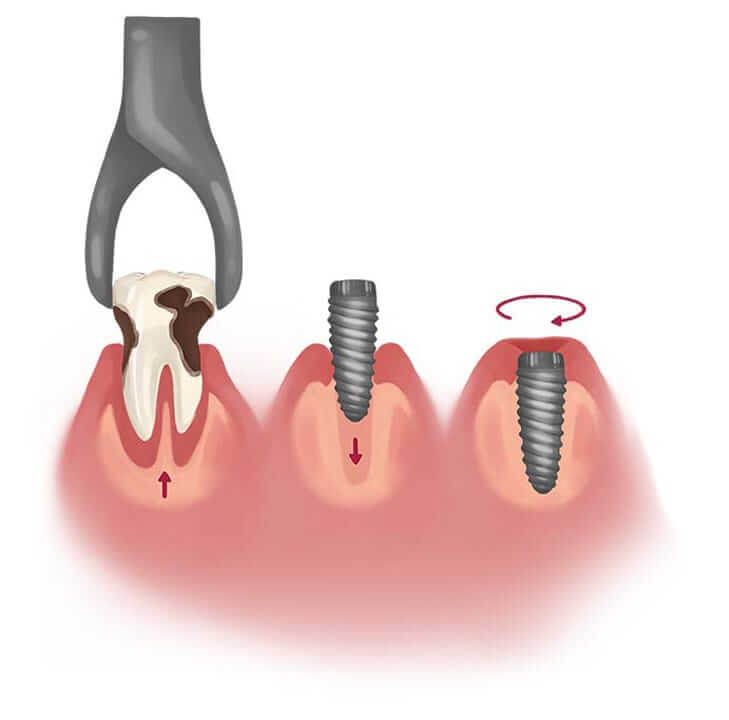
- Tooth Extraction (If Necessary): If you have damaged or decayed teeth that need to be removed before implant placement, tooth extraction may be performed as a preliminary step. In some cases, immediate implant placement can be done at the same time as tooth extraction, while in others, a healing period may be necessary before implant surgery.
- Implant Placement Surgery: The implant placement surgery is typically performed under local anesthesia or sedation to ensure your comfort throughout the procedure. Using precise surgical techniques, your dentist or oral surgeon will create an incision in the gum tissue to access the underlying jawbone. A series of specialized drills will then be used to prepare the bone for implant placement. Once the implant site is prepared, the endosteal implant is carefully inserted into the jawbone and positioned for optimal stability and aesthetics.
- Healing and Osseointegration: After implant placement, a healing period is necessary to allow the implant to integrate with the surrounding jawbone—a process known as osseointegration. During this time, the bone tissue gradually fuses with the surface of the implant, providing a strong and stable foundation for the eventual attachment of prosthetic teeth. Healing times vary depending on factors such as bone quality, implant location, and individual healing response, but typically range from several weeks to a few months.
- Abutment Placement: Once osseointegration is complete, a second minor surgical procedure may be performed to place abutments—small connectors that protrude from the top of the implants and serve as attachment points for the final prosthetic teeth. Abutment placement is usually done under local anesthesia, and the gum tissue is allowed to heal around the abutments for a few weeks before the final restoration is attached.
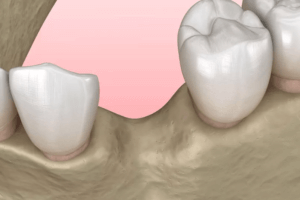
- Prosthetic Tooth Placement: The final step in the implant process involves attaching the prosthetic teeth to the abutments. These may include individual crowns for single-tooth replacements, bridges for multiple adjacent teeth, or implant-supported dentures for full arch restorations. The prosthetic teeth are custom-designed to match the size, shape, and color of your natural teeth, providing a lifelike and aesthetic result.
- Follow-Up and Maintenance: After the completion of implant treatment, regular follow-up visits with your dentist are essential to monitor the health and function of your implants and prosthetic teeth. Routine oral hygiene practices, including brushing, flossing, and professional cleanings, are also crucial for maintaining the longevity and success of your implants.
By following these steps and working closely with your dental team, you can achieve a restored smile and optimal oral function with endosteal dental implants. Each stage of the process is carefully planned and executed to ensure the best possible outcome for your long-term dental health and well-being. If you have further questions about Endosteal Dental Implant, please contact us.
How Long Does Endosteal Dental Implant Last?
Endosteal dental implants are designed to be a permanent tooth replacement solution, offering exceptional durability and longevity when properly cared for. While individual experiences may vary depending on factors such as oral hygiene, overall health, and lifestyle habits, endosteal implants can last for many years or even a lifetime with the following considerations:
- Osseointegration: The success and longevity of endosteal implants depend on the process of osseointegration—the integration of the implant with the surrounding jawbone. Proper osseointegration ensures that the implant becomes a stable and functional part of your oral anatomy, providing a strong foundation for prosthetic teeth. Following implant placement, it typically takes several months for osseointegration to occur fully.
- Oral Hygiene: Maintaining good oral hygiene is essential for the long-term success of endosteal implants. Brushing at least twice a day, flossing daily, and using antimicrobial mouthwash can help prevent plaque buildup and reduce the risk of peri-implantitis—a condition characterized by inflammation and infection around the implant. Regular dental check-ups and professional cleanings are also crucial for monitoring implant health and detecting any potential issues early on.
- Lifestyle Factors: Certain lifestyle habits, such as smoking, excessive alcohol consumption, or poor dietary choices, can negatively impact implant longevity. Smoking, in particular, has been associated with increased rates of implant failure and complications due to impaired healing and decreased blood flow to the gums and jawbone. Adopting a healthy lifestyle and avoiding harmful habits can contribute to the long-term success of your implants.
- Bite Force and Occlusion: Proper occlusion (bite alignment) is essential for distributing biting forces evenly across the implant-supported prosthetic teeth and minimizing stress on the implants. Patients with bruxism (teeth grinding) or malocclusion (misaligned bite) may be at higher risk of implant complications if these issues are not addressed. Your dentist may recommend wearing a night guard or orthodontic treatment to correct bite abnormalities and protect your implants.
- Regular Maintenance: Routine maintenance and follow-up care are key to preserving the longevity of endosteal implants. Your dentist will schedule regular check-ups to monitor the health and stability of your implants and prosthetic teeth. Any signs of implant-related complications, such as gum inflammation, mobility, or discomfort, should be promptly addressed to prevent further problems and ensure the longevity of your implants.
With proper care and maintenance, endosteal dental implants can provide a reliable and long-lasting solution for replacing missing teeth and restoring oral function. By following your dentist’s recommendations and practicing good oral hygiene habits, you can maximize the lifespan of your implants and enjoy a healthy, functional smile for years to come. If you have further questions about Endosteal Dental Implant, please contact us.
What Are Common Problems With Endosteal Dental Implant?
While endosteal dental implants are generally safe and successful for most patients, like any dental procedure, they may be associated with certain complications or problems. Understanding these potential issues can help you recognize and address them early on. Here are some common problems that may occur with endosteal dental implants:
- Peri-Implantitis: Peri-implantitis is a condition characterized by inflammation and infection of the tissues surrounding the implant, similar to periodontal disease around natural teeth. It is often caused by plaque accumulation around the implant site, leading to gum inflammation, bone loss, and eventual implant failure if left untreated. Regular oral hygiene practices and professional cleanings are essential for preventing peri-implantitis.
- Implant Failure: While relatively rare, implant failure can occur due to various factors, including inadequate osseointegration, infection, peri-implantitis, or mechanical complications. Signs of implant failure may include mobility, pain, discomfort, or visible changes in the gum tissue surrounding the implant. Prompt evaluation and treatment by your dentist are necessary to address implant failure and prevent further complications.
- Soft Tissue Complications: Soft tissue complications, such as gum recession, mucositis (inflammation of the gum tissue), or inadequate keratinized tissue around the implant, can affect the aesthetics and health of the implant site. Proper management of soft tissue contours and maintenance of adequate keratinized tissue can help prevent complications and ensure optimal implant esthetics and stability.
- Mechanical Problems: Mechanical problems with the implant components, such as loosening or fracture of the abutment or prosthetic screws, may occur over time. These issues can compromise the fit and function of the prosthetic teeth and may require repair or replacement of the affected components. Regular dental visits and routine maintenance of implant restorations are essential for detecting and addressing mechanical problems early on.
- Nerve Injury: During implant surgery, there is a risk of nerve injury, particularly in the lower jaw where the inferior alveolar nerve runs. Nerve damage may result in numbness, tingling, or altered sensation in the lips, chin, or tongue. While nerve injuries are rare, they can cause temporary or permanent discomfort and may require additional treatment to resolve.
- Aesthetic Concerns: Aesthetic concerns, such as mismatched color, shape, or size of the prosthetic teeth, or visible metal components in the restoration, may arise following implant placement. Proper planning and communication with your dentist during the treatment planning phase can help ensure that the final restoration meets your aesthetic expectations and blends seamlessly with your natural smile.
If you experience any problems or complications with your endosteal dental implants, it’s essential to contact your dentist promptly for evaluation and treatment. Early intervention can help prevent further complications and ensure the long-term success of your implant therapy. If you have further questions about Endosteal Dental Implant, please contact us.
We also think you’ll like…
Dental Bone Loss
Dental Bone Loss What Is Dental Bone Loss? Dental bone loss, also known as periodontal bone loss or alveolar bone loss, refers to the loss

Titan Dental Implants
Titan Dental Implants What Are Titan Dental Implants? Titan is a dental implant company that specializes in providing innovative solutions for dental implantology and oral

Neoss Dental Implants
Neoss Dental Implants What Are Neoss Dental Implants? Neoss is a dental implant company that specializes in providing innovative solutions for dental implantology and oral

Bone Graft Post-Operative Instructions
Bone Graft Post-Operative Instructions What You Should Do After Your Dental Bone Graft Surgery Alveolar bone preservation is a dental procedure that involves placing a bone

Megagen Dental Implants
Megagen Dental Implants What are Megagen Dental Implants? Megagen is a prominent player in the field of dental implantology, known for its innovative approach to

Osstem Dental Implants
Osstem Dental Implants What Are Osstem Dental Implants? Osstem is a prominent South Korean dental implant company that has made significant strides in the field

